What is Oropharyngeal Cancer?
Oropharyngeal cancer, also known as tonsil cancer, is a disease in which abnormal cells with the potential to both grow locally and spread to other parts of the body are found in the tissue of the part of the throat (oropharynx). This includes the base of the tongue, the tonsils, the soft palate, and the walls of the pharynx. In my case, the soft palate and pharynx are not involved.
https:/
Testing and Diagnosis
A CT scan with contrast showed a tumor on the tonsil approximately 2.9 x 2.1 x 3.0 cm, a slightly smaller tumor on the base of tongue, and a partially cystic mass within the right level II region, approximately 3.6 x 2.9 x 3.2 cm in size, located at the anterior margin of the right sternocleidomastoid muscle. The mass was believed to be metastatic adenopathy.
Thus, the tentative diagnosis was Stage III if HPV+.
A fine needle aspiration with ultrasound guidance was performed on the lymphatic cyst, but the analysis was inconclusive due to insufficient cancerous cells in the fluid.
A surgical biopsy was performed on the base of tongue under general anesthesia. This time, the analysis confirmed it was HPV+ P16 cancer.
Finally, a PET-CT scan was performed to confirm the size and location of cancerous tissues, and to identify any potential remote metastases, of which none were seen.
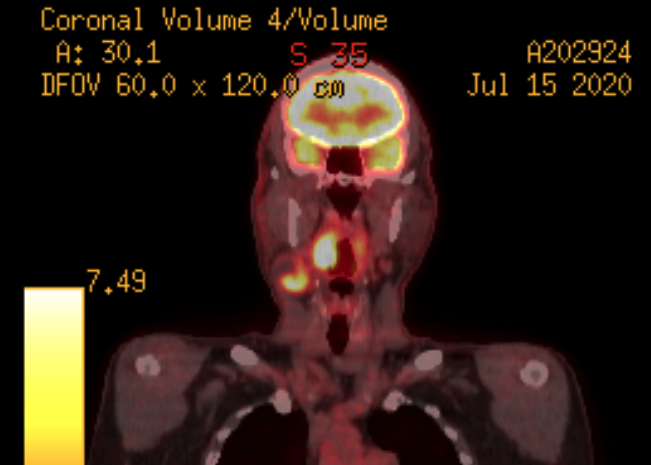
Positron emission tomography (PET) is a nuclear imaging technology that enables visualization of metabolic processes in the body. A radionucleide tracer, in this case fluorodeoxyglucose (FDG) is injected, which the body metabolizes in the same way as normal glucose. When metabolized, the tracer molecules emit a positron which combines with electrons to produce an orthogonal pair of gamma rays, which are detected by a scanner ring. The gamma ray vector data is used to reconstruct a color-mapped 3D image database corresponding to glucose uptake levels. The image shown above is a single 3D “slice” through the suspected cancer area in the head and neck. Glucose “hot spots” are indicated by yellow color mapping. Hot spots appearing in the suspected area indicate cancerous tissue. Areas of the body which are normally high-glycolic such as the brain, eyes, kidneys, and urinary tract also appear as hot spots, but can be safely ignored in this case.
Treatment
My treatment plan consists of a single weekly chemotherapy session plus radiotherapy sessions 5 days per week. The treatment runs for 7 weeks total.
Adjuvant therapies include speech and language pathologist sessions to exercise swallowing muscles, and physical therapy sessions to stretch neck muscles and tissues to reduce stiffness and improve lymph drainage and circulation.
The chemotherapy regimen consists of Cisplatin and other agents delivered intravenously by infusion pump. Other agents include Potassium Chloride, Magnesium Sulfate, and Sodium Chloride IV 0.9 % for electrolytes and hydration, corticosteroids Dexamethasone and Methylprednisolone to prevent inflammation, Diphenhydramine to suppress allergic reaction, and Fosaprepitant and Palonosetron to prevent vomiting. The weekly chemo infusion takes about 6 hours.
Radiotherapy sessions are delivered on a Varian TrueBeam Linear Accelerator. This sophisticated IMRT (Intensity Modulated Radiation Therapy) machine produces a dynamically modulated and collimated ionizing radiation beam while moving circumferentially around the patient. A tungsten multi-leaf collimator shapes the beam cross section to produce a precisely targeted high radiation dose in the cancerous tissue while minimizing the radiation dose delivered to surrounding healthy tissues. An integrated CT scanner precisely determines patient position and orientation to achieve repeatable sub-millimeter positional accuracy.
Each daily radiotherapy session is painless and takes less than 15 minutes. The overall cumulative dose is 70Gy for the 3 targeted cancerous areas, 40Gy for the overall neck, with minimized dose on salivary glands, thyroid, etc. The daily fractionated dose is about 2Gy.
Expected Side Effects of Treatment
- Permanent:
- xerostomia (loss of overall salivary output)
- loss of right submandibular salivary gland
- loss of lower right molars requiring partial denture
- Temporary:
- oral mucositis (inflamed mucous membranes)
- changes in smell and taste (can be permanent)
- intense pain in high dose irradiated areas, increasing from treatment start, subsiding 2-3 weeks post-treatment
- intense referred pain in right ear (tympanic nerve bundle overload), lasting from pre-treatment until approximately 2 weeks post-treatment
Medications
- Amlodipine – blood pressure (unrelated to cancer)
- Tylenol 500mg – pain management
- Oxycodone 5mg – pain management
- Fentanyl patch – pain management
Follow-up and Prognosis
Post treatment follow up PET scans will be done at 1 month to confirm reduction of cancerous tissue, 3 months to assess healing and/or recurrence, 6 months to assess healing and/or recurrence. PET scan will be performed 2x yearly until disease free for 5 years.
5-year overall survival rate is 90%.